Bone Health at Menopause: What You Need to Know Beyond Calcium
Bone health at menopause is a major concern for many women around 50. This natural phase brings hormonal shifts — particularly a drop in oestrogen — that can accelerate bone density loss and raise the risk of osteoporosis, an inflammatory condition that weakens bones and increases fracture risk.
While hormone replacement therapy (HRT) is often suggested as the primary way to support bones, nutrition and lifestyle choices play a crucial role too. A functional approach considers all factors that influence bone strength, not just oestrogen or calcium.
Why Menopause Affects Bone Health
Women reach their peak bone mass around 25 to 30 years old, when bones are strongest. Oestrogen helps maintain this strength, so as levels decline during menopause (around age 50 on average), bone loss speeds up. If your peak bone mass wasn’t ideal, this loss can lead to osteoporosis — about one in two women over 60 will experience a fracture related to it.
The Role of a Varied, Nutrient-Rich Diet
Building and maintaining bone requires a wide range of nutrients working together. Antioxidants like vitamin C and carotenoids (plant-based vitamin A), phytoestrogens such as those found in soya, and compounds like lycopene in tomatoes and cherry extract have all been shown to support bone health.
Dairy often gets the spotlight because of its calcium content, but it only offers about 30% calcium absorption. Some leafy greens have less calcium but better absorption rates (around 50%), so foods like cooked bok choy can provide similar benefit. Oxalates in some vegetables can bind calcium, but there are plenty of options to include.
Calcium: Essential but Not in Isolation
Calcium is vital, but more isn’t always better. Too much calcium from supplements (above 2000mg per day) may raise heart risks due to artery calcification. The research isn’t conclusive, but food sources are safer as the body regulates absorption naturally.
For women over 50, a daily total of around 1200mg calcium (including food and supplements) is recommended. Good sources include dairy, leafy greens, tofu, nuts like almonds, and fermented foods that aid absorption. Calcium’s best effects come alongside other nutrients
Key Nutrients for Strong Bones
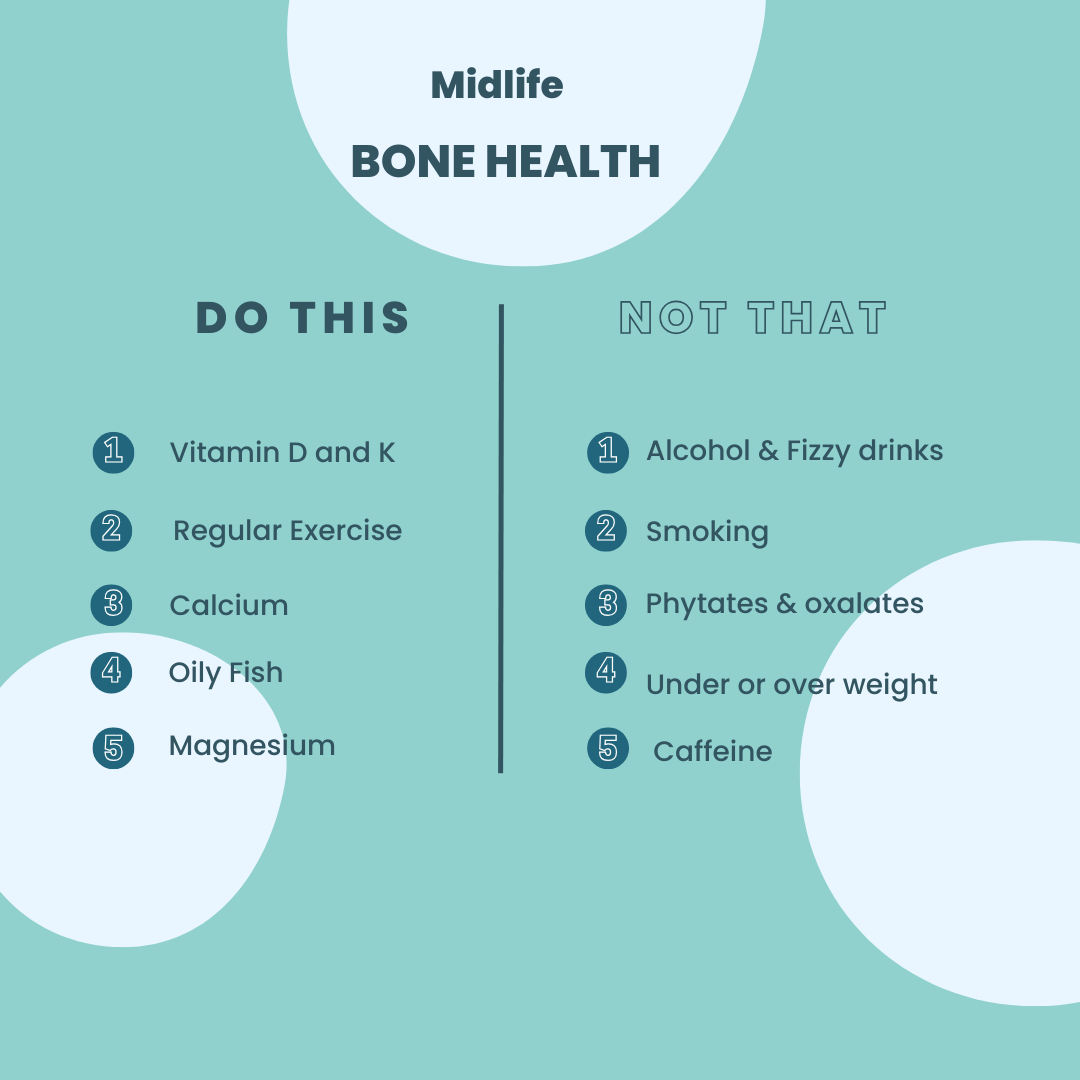
- Vitamin D — Helps your body absorb calcium. Aim for 800-1000 IU daily, from sun exposure, fatty fish, egg yolks, or fortified foods.
- Magnesium — Regulates calcium levels and supports bone structure. Found in nuts, seeds, whole grains, and greens.
- Vitamin K — Activates proteins essential for bone metabolism. Leafy greens, cruciferous vegetables, fermented foods, and certain animal products like liver and eggs are rich sources.
- Omega-3 Fatty Acids — Reduce inflammation that can accelerate bone loss. Fatty fish, flaxseed, chia seeds, olive oil, and avocado oil are excellent choices.
In addition to a healthy diet supplements can be targeted to support bone health. I always advise getting professional advice as there are many factors to consider from the quality of supplements to the medications you take.
Watch What Could Hinder Calcium Absorption
- Caffeine — Can increase calcium loss in urine, but moderate intake (especially with milk added) and tea’s beneficial flavonoids may mitigate effects.
- Salt and Excess Vitamin A — High salt diets and certain forms of vitamin A (like those in organ meats and fish liver oil) can reduce calcium absorption.
- Soft Drinks — High phosphoric acid content disrupts calcium/phosphorus balance, linked to decreased bone density and fracture risk.
- Anti-nutrients — Compounds like phytates, lectins, and oxalates in some plant foods can bind minerals and reduce absorption. Soaking, sprouting, fermenting, and cooking methods can reduce these effects.
If your digestion isn’t optimal, these factors may have a bigger impact. Supporting gut health is an important part of preserving nutrient absorption.
Lifestyle Habits to Protect Your Bones
- Regular weight-bearing exercise (walking, running, resistance training) strengthens bones. Aim for 30 minutes most days.
- Limit alcohol and caffeine as both can encourage bone loss. Keep alcohol to one drink daily and caffeine to 2-3 cups of coffee.
- Quit smoking, which weakens bone density and increases osteoporosis risk.
- Maintain a healthy weight — being under- or overweight raises bone loss risk.
A Functional Approach for Long-Term Bone Health
Each woman’s bone health journey is unique. A functional medicine and nutritional therapy approach looks beyond symptoms, addressing root causes including diet, lifestyle, digestion, and hormonal balance.
If you’re concerned about your bone health or want tailored nutritional support, I offer a various options. A good starting point is a The Midilfe Nutrion Reboot Where I assess your diet and nutrient intake, and provide step by step approach to adjusting your diet with personalised recommendations.
References
Chen L, Liu R, Zhao Y, Shi Z. High Consumption of Soft Drinks Is Associated with an Increased Risk of Fracture: A 7-Year Follow-Up Study. Nutrients. 2020 Feb 19;12(2):530. doi: 10.3390/nu12020530. PMID: 32092922; PMCID: PMC7071508.
Sahni S, Mangano KM, McLean RR, Hannan MT, Kiel DP. Dietary Approaches for Bone Health: Lessons from the Framingham Osteoporosis Study. Curr Osteoporos Rep. 2015 Aug;13(4):245-55. doi: 10.1007/s11914-015-0272-1. PMID: 26045228; PMCID: PMC4928581.
The Royal Osteoporosis Society March 2021 Sarah Leyland, https://theros.org.uk/blog/2021-03-22-what-s-the-menopause-got-to-do-with-bone-health/
Shieh A, Ruppert KM, Greendale GA, Lian Y, Cauley JA, Burnett-Bowie SA, Karvonen-Guttierez C, Karlamangla AS. Associations of Age at Menopause With Postmenopausal Bone Mineral Density and Fracture Risk in Women. J Clin Endocrinol Metab. 2022 Jan 18;107(2):e561-e569. doi: 10.1210/clinem/dgab690. PMID: 34537850; PMCID: PMC8764341.