Are you stressed out?
It’s almost a badge we are proud of in our culture. In a human context it was unheard of until the late 1940’s, when the term was used for people not metal testing in engineering! The world has changed with a busier pace of life, more technology more methods of communication, we have a different type of stress these days. Recent pandemic lockdown has added to mental health problems due to isolation, bereavement, economic pressures or family frictions. This has brought a new focus on mental well being. Humans are designed for survival unfortunately our culture and lifestyle doesn’t accommodate this causing the stress response to be sustained. The Chronic activation of this survival mechanism impairs health. In menopause this is exacerbated by the interplay of stress and sex hormones. (1) The good news is there are a lot of lifestyle changes that we can use to support our resilience.
Acute Stress
Stress is perceived in the senses, eyes and ears which send the information to the amygdala, an area of the brain for emotional processing which sends a distress signal to the hypothalamus area which is like a command centre communicating with the rest of the body through the nervous system.(2) Acute stress is comes and goes quickly, so if you are late and running to catch a bus this will cause he sympathetic nervous system (SNS) to tell the adrenals glands above the kidneys to release hormones adrenalin (epinephrine) and cortisol to be released this quickly activates the body system to deal with the stress. These hormones act together to direct the nervous system and cause the heart to beat faster, respiration rate to increase, blood vessels in the arms and legs to dilate, digestive process to change and glucose levels (sugar energy) in the bloodstream to increase to deal with the emergency. The SNS response is for emergencies in the short term a bit like pressing the accelerator in a car.
If the brain continues to perceive something as dangerous the hypothalamus activates the second part of the stress response, the HPA axis, consisting of the hypothalamus, the pituitary gland, and the adrenal glands. The HPA axis uses hormonal signals to keep the SNS activated, like pressing the accelerator down, the hypothalamus releases corticotropin-releasing hormone (CRH), which travels to the pituitary gland, triggering the release of adrenocorticotropic hormone (ACTH) stimulating the adrenal glands to release cortisol. The body can stay on high alert.
Once the crisis is over, cortisol levels fall, the PNS acts as the brake that dampens the stress response and the body returns to the unstressed state. This recovery is facilitated by the parasympathetic nervous system (PNS) which mostly has opposing effects to the SNS. Both the SNS and the PNS have powerful interactions with the immune system, which can also influence the stress response. (3)
Immune disadvantage
When we are stressed, the immune system’s ability to fight off ‘foreign invaders’ (antigens) is reduced causing us to be more susceptible to infections. The corti-costeroids (stress hormones) suppress the efficiency of the immune system, lowering the number of immune cells. Normally Cortisol is responsible for turning off the stress response via complex immune processes however this can malfunction in chronic stress. See other Immunity Blogs
Chronic stress will also lead to health problems because of the effect of sustained stress hormones on the body. For example, raised blood sugar and blood pressure may lead to diabetes and heart disease. Stress also produces an increase in cholesterol levels, due to more energy being made in the form of fatty acids so the liver produces more of the bad cholesterol, LDL.
Chronic Stress
In the past stress would have been hunting down your dinner or running away form an enemy to save your life! The immediate risk of death is full on stress but if you lived your stress response would subdue quickly once the incident was over. Since we are wired for survival the body can also overreact to ‘modern’ stressors that are not life-threatening, such as traffic jams, work pressure, and relationships in addition our pace of life is fast, mobile phones mean we are always available, emails, social media, make extra demands for our attention. This means we are more likely to suffer the effects of sustained stress response. (4)
Under chronic stress cortisol production can malfunction referred to as cortisol resistance. Hormones work like a lock and key however if there are surplus hormones the cells receptors become blunted in their response (as a safety mechanism). So when excess cortisol is in our system it knocks on the cell receptor door but they don’t let it in. it’s vicious cycle as more cortisol will then be made resulting in less physiological resilience to stress. (5)
Menopause Stress
So how does this affect women in the peri menopause or post menopause. Evidence is lacking as menopause itself exerts stress on the mind and body, so studies often interlink the two. It is more widely recognised that menopause interferes with cognition, sleep, temperature control and blood sugar all of which have a relationship with our hormonal system! What is clear is that stress has huge impact on our bodies. Menopause will add to both physiological and psychological stress.(6)
The Adrenals
The adrenal glands small gland like a hat on the kidneys! This where corticosteroids are produced. They have a new role to produce sex hormones during menopause transition. However, current or built up stress can deplete the adrenal glands and inhibit their ability to produce sex hormones. This is sometimes referred to as ‘adrenal fatigue’ not proven by science. (7)
“The term “adrenal fatigue” has been used to explain a group of symptoms that are said to occur in people who are under long-term mental, emotional, or physical stress.”- hormone.org.’
Symptoms include fatigue, low mood, weight gain, irritability, increased pre-menstrual syndrome, Sleep difficulties, Heavy bleeding/irregular bleeding, Headaches, Hot flushes (8)and night sweats, Vaginal dryness, Skin changes, Urinary incontinence, Joint pain/stiffness.
If this sounds familiar, then it yes perimenopause and adrenal dysfunction have similar symptoms and likely overlap. The pituitary gland influences both via the hypothalamus, which in turn directs hormone production by the ovaries and the adrenal glands.
Factors that impact hormone balance
- The stress response can take over and push aside sex hormone production. This Causes symptoms similar to menopause e.g poor sleep, anxiety, depression. Many women recognise menopause symptoms worsen during stress
- Environmental factors, endocrine disruptors, chemicals and other pollutant.
- Current or built up stress can deplete the adrenal glands and inhibit their ability to make sex hormones.
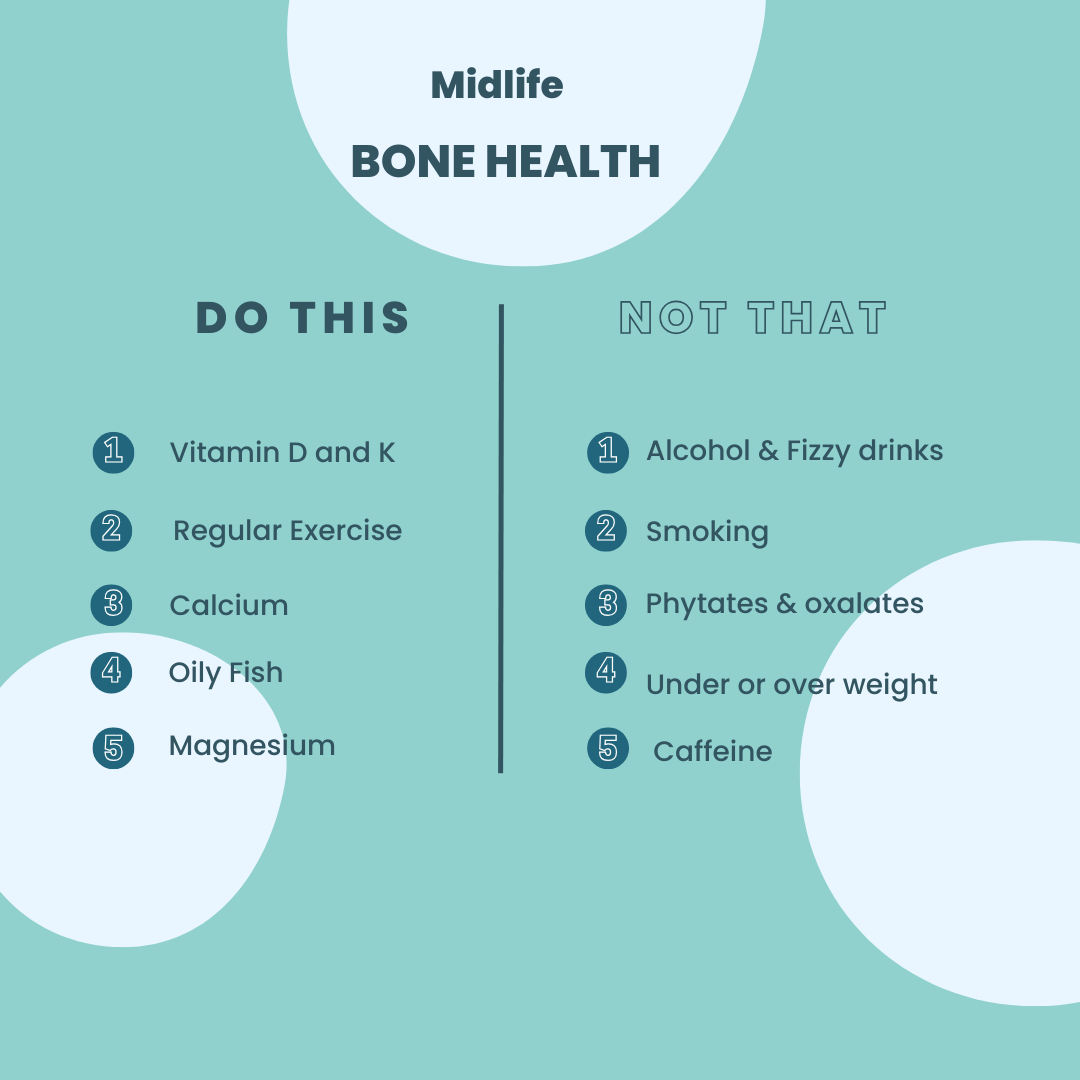
- Stress robs us of key nutrients required for hormone productions and clearance e.g Magnesium, zinc, B vitamins.(9)
- Gut bacterial balance is affected by oestrogen and stress. This can hamper sex hormone binding globulin SHBG that helps usher sex hormones around the body. (3)
Top Tips to Reduce Stress
- What’s causing the stress? Is it a person or a task and write it down.
- Tick off what you can change, e.g. planning, taking a break, a healthy lunch
- Prioritise so important things happen. This includes rest, fun and social life.
- Learn to say NO When commitments don’t fit your priorities!
- See the signs of stress, stiff neck, headache, anxiety? Take action with a brief change in activity. Stretching is great!
- Look after yourself, a healthy body can cope with stress but more importantly learn to reduce it. Get sleep, exercise and good food.
- Importantly ‘The Stress’ isn’t the issue or the relative, boss or big task it’s your reaction to it and how you cope with it.
To find out how I can help you with menopause concerns book a no obligation Discovery call
- Hardy C, Thorne E, Griffiths A, Hunter MS. Work outcomes in midlife women: the impact of menopause, work stress and working environment. Women’s Midlife Health [Internet]. 2018 Dec 9 [cited 2020 Oct 9];4(1):3. https://womensmidlifehealthjournal.biomedcentral.com/articles/10.1186/s40695-018-0036-z
- Mariotti A. The effects of chronic stress on health: new insights into the molecular mechanisms of brain-body communication. Future science OA [Internet]. 2015 Nov [cited 2019 May 25];1(3):FSO23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28031896
- Joseph D, Whirledge S, Joseph DN, Whirledge S. Stress and the HPA Axis: Balancing Homeostasis and Fertility. International Journal of Molecular Sciences [Internet]. 2017 Oct 24 [cited 2019 May 20];18(10):2224. Available from: http://www.mdpi.com/1422-0067/18/10/2224
- Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: A review. EXCLI journal [Internet]. 2017 [cited 2019 May 25];16:1057–72. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28900385
- Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proceedings of the National Academy of Sciences of the United States of America [Internet]. 2012 Apr 17 [cited 2020 Oct 9];109(16):5995–9.
- Alexander JL, Dennerstein L, Woods NF, McEwen BS, Halbreich U, Kotz K, et al. Role of stressful life events and menopausal stage in wellbeing and health. Expert Review of Neurotherapeutics [Internet]. 2007 Nov 9 [cited 2019 May 20];7(sup1):S93–113. Available from: http://www.tandfonline.com/doi/full/10.1586/14737175.7.11s.S93
- Morley JE, Perry HM. Androgens and women at the menopause and beyond [Internet]. Vol. 58, Journals of Gerontology – Series A Biological Sciences and Medical Sciences. Gerontological Society of America; 2003 [cited 2020 Oct 9]. p. 409–16. Available from: https://academic.oup.com/biomedgerontology/article/58/5/M409/536121
- Schreiber DR, Dautovich ND. Depressive symptoms and weight in midlife women: The role of stress eating and menopause status. Menopause [Internet]. 2017 Oct 1 [cited 2020 Oct 9];24(10):1190–9.
- Hodges RE, Minich DM, Biesalski HK. Modulation of Metabolic Detoxification Pathways Using Foods and Food-Derived Components: A Scientific Review with Clinical Application. 2015; Available from: http://dx.doi.org/10.1155/2015/760689